Real Humans.
Real Conversations.
Real Results.
86Borders is a human-first care coordination and member engagement company that helps health plan members overcome obstacles to care — especially among hard-to-reach populations.

More than engagement. Real connections.
Unlike transactional outreach solutions that rely on mass texts, voicemails, or AI scripts, 86Borders builds trusted relationships that lead to measurable outcomes. Our locally based Care Coordinators meet members where they are, while the ConnectAllCare platform ensures every interaction is backed by supportive technology and actionable insights.

Human Touch
Locally based coordinators,
not call centers.

Technology that Amplifies
ConnectAllCare platform integrates with plan workflows.

Real Outcomes
Improved Star Ratings, closed HEDIS® gaps, reduced ER/IP visits, improved RAF.
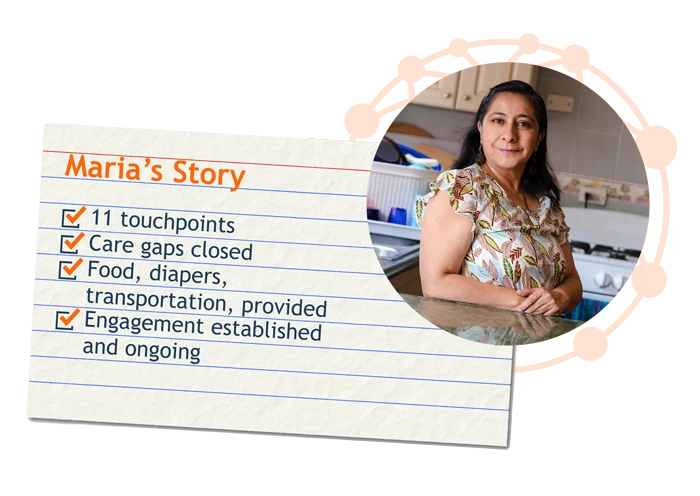
Real stories. Real results.
When health plans couldn’t reach Maria, a D-SNP member with multiple chronic conditions, 86Borders stepped in. In just 26 days, with 11 interactions, our Spanish-speaking Care Coordinator engaged Maria and built trust, addressed her social needs, closed critical gaps, and kept her engaged in her care.
Human-first. Technology-enabled. Outcomes-focused.
Our model combines the empathy of Care Coordinators with the intelligence of ConnectAllCare:

Engage and Activate:
Real conversations that spark trust.

Address Social Needs:
Food, housing, transportation, and more.

Close Gaps in Care:
From annual visits to medication adherence.

Track Results:
Not just contact metrics — outcomes that matter.
Serving every population that health plans struggle to reach.
Medicare Advantage
Medicaid
D-SNP
Exchange
Veterans
“86Borders has made a significant positive impact on our efficiency and quality scores and kept appointments.”
Medical Director, Patient Centered Medical Home Group
Real Results
Outcomes proven at scale.
%
D-SNP Statin Adherence Conversions for Non-Compliant List
in MA/DSNP Plan
%
Reduction in Total Cost of Care in Medicaid Plan
%
Reduction in Inpatient/ER Utilization in Medicaid Plan
+1
+1
Star Improvement in all 3 Med Adherence Measures for
MA/D-SNP Plan
%
Intervention Rate for HEDIS® SNS-E in Exchange Plan
%
Increase in Colorectal Cancer Screening in Exchange Plan

Let’s redefine engagement and make a difference, together.
Real humans, real conversations, and real results — that’s how 86Borders delivers value for health plans and the members they serve.